Practice Essentials
Medial epicondylitis, also called golfer's elbow, was first described in 1882 by Henry J Morris. [1] This condition is an overuse syndrome that is characterized by pain at the flexor-pronator tendinous origin and is seen in sports activities with repetitive valgus stress, flexion, and pronation, such as occurs in golf, baseball, tennis, fencing, and swimming. [2] This condition is also seen with occupations that require hand, wrist, and forearm motions. [3, 4, 5, 6]
The flexor carpi radialis (FCR) and the pronator teres are commonly involved at the insertion of the medial epicondyle; however, the flexor digitorum superficialis (FDS) and the flexor carpi ulnaris (FCU) are less likely to be involved. Ulnar neuropathy may be associated in approximately 50% of cases. [7]
Conservative therapy includes activity modification, administration of nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroid injections (see Treatment). [8] Surgical treatment should be considered in cases where conservative treatment has failed after 6-12 months and after all other pathology has been excluded.
Anatomy
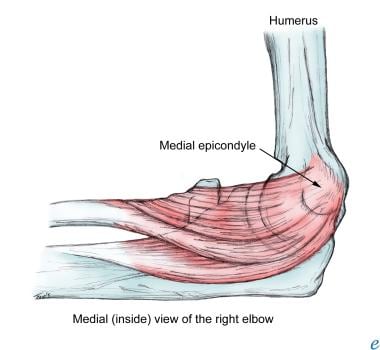
The ulnar (or medial) collateral ligament (UCL) and the radial (or lateral) collateral ligament (RCL) are the elbow stabilizers. The UCL is the primary valgus stabilizer, and the RCL is the primary varus stabilizer. (See the image below.)
The UCL plays a very important role in the surgical treatment for medial epicondylitis and is composed of three parts, as follows:
-
Anterior oblique ligament (AOL) and accessory AOL (medial conjoint tendon [MCT])
-
Posterior oblique ligament (POL)
-
Transverse ligament
The muscles involved in medial epicondylitis primarily include the pronator teres and the FCR. Less likely to be involved are the palmaris longus, the FDS, and the FCU.
The anterior medial epicondyle is the primary area of involvement with this condition. The pronator teres partially originates from the superoanterior medial epicondyle, but its primary origin is from the MCT. The AOL is an important valgus stabilizer that must be preserved during surgical intervention. [7] The AOL lies on the posterior margin of the MCT; therefore, the MCT should be located and explored with caution to avoid injury to the AOL. [7] The MCT is not a valgus stabilizer and can be removed if the AOL is intact.
The second most commonly involved muscle is the FCR, which also has a primary origin from the MCT, with a small area of origin from the medial epicondyle. The MCT serves as an important surgical landmark for identification of the involved muscles and in the avoidance of the AOL. [7]
It is important to review the anatomic landmark of the ulnar nerve and the medial antebrachial cutaneous nerve (MACN) before proceeding with any surgical procedure. At the elbow, the ulnar nerve enters the ulnar groove between the medial epicondyle and the olecranon process. The MACN is in the subcutaneous tissue just proximal to the medial epicondyle, where it divides into the anterior and posterior branches. The posterior branch travels directly over the flexor pronator mass to the posterior medial forearm. [9]
Pathophysiology
Originally, inflammation was thought to generate the pain in medial epicondylitis. However, magnetic resonance imaging (MRI) and histology show the presence of microtears in the flexor-pronator tendons without inflammation. In addition, histologic evaluation following surgical treatment has revealed angiofibroblastic hyperplasia and fibrillar degeneration of collagen. [10] Nirsch spoke of "tendinosis" and "angiofibroblastic degeneration" in describing the pathophysiology of medial epicondylitis as microtears in the tendon with a poor healing response. [11] An acutely inflammatory component may be seen, but the tendon may degenerate over weeks to months.
Zeisig et al reported evidence of local, nonneuronal production of catecholamines, but not acetylcholine, in fibroblasts in the tissue at the muscle origin at the lateral epicondyles in patients with tennis elbow and the medial epicondyles in patients with golfer's elbow. Tyrosine hydroxylase-like immunohistochemical reactions were seen in fibroblasts in four of seven patients with tennis elbow and in two of four with golfer's elbow. No such reactions were detected in the six healthy, asymptomatic control patients. According to the authors, the presence of catecholamines may have an influence on blood vessel regulation and pain mechanisms in these conditions. [12]
Epidemiology
In the United States, medial epicondylitis is reported to be the most common cause of medial elbow pain. However, it is less common than lateral epicondylitis (tennis elbow). [13] There is a sex predilection for men, with a male-to-female ratio 2:1. The peak incidence of this condition is noted to be between the third and fifth decades of life.
The dominant elbow is involved in approximately 60% of cases, and 30% of patients have an acute onset, with 70% having an insidious onset. [7] In a cross-sectional study of about 10,000 randomly selected adults, 11% reported elbow pain in the previous week. Of those surveyed, 0.6% were diagnosed with medial epicondylitis. [14]
Prognosis
Poor prognostic factors for medial epicondylitis include work activities with high levels of strain, particularly with nonneutral wrist postures. [15]
Cho et al reported the results of miniopen muscle resection for intractable lateral or medial epicondylitis in 42 elbows following 6 months of conservative treatment, a history of more than three steroid injections, or severe functional impairment. [16] Average preoperative visual analogue scale (VAS) scores of pain were 5.36 at rest, 6.44 at daily activities, and 8.2 at sports or occupational activities. After surgery, the VAS scores were 0.3 at rest, 1.46 at daily activities, and 2.21 at sports or occupational activities.
Preoperative Roles and Maudsley scores were acceptable in 6 cases and poor in 36 cases; postoperative scores were excellent in 23 cases, good in 16 cases, and acceptable in three cases. [16] Overall, 41 cases (97.6%) achieved satisfactory results. Postoperative complications consisted of two cases of subcutaneous seroma due to leakage of joint fluid, which was successfully managed by additional surgery and suction drainage.
Shahid et al conducted a retrospective study to assess outcomes of open surgery for patients with recalcitrant medial epicondylitis following failed conservative management. [17] The investigators reviewed clinical results for 15 patients (17 elbows). The mean follow-up period of the study cohort was 66 months.
In this study, operative treatment improved patient function significantly. [17] There was a mean increase of 10 kg in grip strength and a mean decrease (improvement) of 25.7 in the Disabilities of the Arm, Shoulder and Hand (DASH) score. All but one patient experienced little or no residual elbow discomfort and had excellent Mayo elbow performance scores postoperatively. Eleven of the 12 patients who were previously employed were able to return to work within 8 weeks of surgery.
Han et al studied 55 patients with 63 cases of medial epicondylitis that were treated surgically after failure of conservative treatment and followed for more than 5 years. [18] Results included the following:
-
Mean VAS score - Improvement from 8.5 to 2.4
-
Nirschl and Pettrone grades - Excellent, 43%; good, 51%
-
Mayo elbow performance scores - Improvement from 72 to 88
-
DASH scores - Improvement from 57 to 23
-
Mean grip strength of the affected side - Improvement from 30 lb to 43 lb
-
Mean time to return to work, 2.8 months; mean time to exercise, 4.8 months
Arevalo et al systematically reviewed the outcomes of 16 studies addressing three surgical approaches to treatment of medial epicondylitis in 479 elbows: open (13 studies), arthroscopic (two studies), and percutaneous (one study). [19] Success rates were in the range of 63-100%, and the complication rate was low, at 4.3%. The rate of return to sports was 81-100%, and that of return to work was 66.7-100% (only one study reported a return-to-work rate lower than 90%). The evidence was insufficient to determine superiority among the three techniques.
Patient Education
The patient should be educated about the condition's contributing factors and activity modification. Increased wrist flexion and pronation should be avoided. If ulnar neuropathy is associated with the medial epicondylitis, the patient should avoid elbow flexion and leaning on the elbow. In addition, in the immediate term, the patient should place ice packs on the medial epicondyle for 10-15 minutes three or four times per day to decrease the inflammation that occurs early in medial epicondylitis.
McCarroll reported that most elbow injuries that are seen during the sport of golf occur during impact. [20] The author recommended that golfers with medial epicondylitis should seek a professional instructor for the proper technique and equipment. Golf-swing modification should begin with a smooth back swing, with the wrist cocking naturally. During the back swing–to–impact transition, motion should begin in the hips to reduce stress in the arms and elbow.
In addition, McCarroll recommended that the forward arm motion should be initiated by the shoulder, not the wrists. The common incorrect swing of casting the club into the swing or hitting from the top can be a major contributor to the development of medial epicondylitis. [20] Moreover, golfers should physically condition themselves to become fit through stretching, strengthening, and cardiovascular exercise before participating in the golf game.
-
Medial epicondyle.