Background
Intrinsic plus hand is a contracture of the intrinsic hand muscles characterized by excessive flexion at the metacarpophalangeal (MCP) joints and extension at the interphalangeal (IP) joints [1] ; it results from imbalance between intrinsic muscles and comparatively weak extrinsic muscles. Contracture of the interosseous, lumbrical, or hypothenar muscles causes the fingers to stiffen and the hand to become deformed and functionally disabled. [2, 3, 4, 5, 6] The frequency of intrinsic plus hand is not known.
The intrinsic plus (or Edinburgh) position has otherwise been known as the safe position for hand splinting. [7] The hand can be immobilized in this position for long periods of time without developing as much stiffness as would occur if the digits were positioned differently. In the intrinsic plus position, the MCP joints are flexed at 60-70°, the IP joints are fully extended, and the thumb is in the fist projection. The wrist is held in extension at 10° less than maximal.
The reason why intrinsic plus is the safe position is that in this position, the MCP joints are in flexion and the IP joints are in full extension. The MCP joints recover well from flexion, and the IP joints recover well from extension on the basis of differences in the shape of the metacarpal head, volar plate, and collateral ligament anatomy (see Anatomy).
Anatomy
Metacarpal head, proximal interphalangeal joints, and collateral ligaments
The metacarpal head is uniquely shaped in that it is ovoid in the sagittal plane, and it widens from the dorsal to the volar dimension. The collateral ligaments are eccentrically mounted dorsal to the axis of rotation of the MCP joint. This anatomy causes variable degrees of tightness on the collateral ligaments based on the position of the joint via a camlike effect. When the joint is in extension, the collateral ligaments are lax. In flexion, the collateral ligaments span a greater distance and are tight (see the image below).
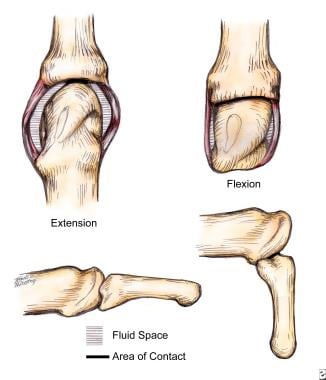 Metacarpal head is uniquely shaped: ovoid in sagittal plane and widening from dorsal to volar dimension. Collateral ligaments are eccentrically mounted dorsal to axis of rotation of metacarpophalangeal joint. This anatomy causes variable degrees of tightness on collateral ligaments based on position of joint via camlike effect. When joint is in extension, collateral ligaments are lax; in flexion, collateral ligaments span greater distance and are tight.
Metacarpal head is uniquely shaped: ovoid in sagittal plane and widening from dorsal to volar dimension. Collateral ligaments are eccentrically mounted dorsal to axis of rotation of metacarpophalangeal joint. This anatomy causes variable degrees of tightness on collateral ligaments based on position of joint via camlike effect. When joint is in extension, collateral ligaments are lax; in flexion, collateral ligaments span greater distance and are tight.
In addition, the MCP joint is curved in two planes to permit abduction, adduction, and rotation, as well as flexion and extension in an abbreviated ball-and-socket configuration. In flexion, bone surface area contact is greater than it is in extension, producing a more stable joint.
Proximal IP (PIP) joint collateral ligaments originate close to the axis of rotation, yielding a smaller change in length with joint position and providing lateral stability. The PIP joint ranges in only one plane, and its trochlear shape also adds to its lateral stability (see the image below).
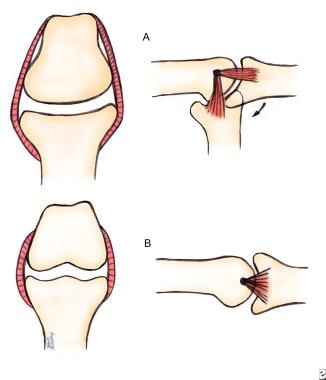 Proximal interphalangeal (PIP) joint collateral ligaments originate close to axis of rotation, providing smaller change in length with joint position and providing lateral stability. PIP joint ranges in only one plane, and its trochlear shape also adds to its lateral stability.
Proximal interphalangeal (PIP) joint collateral ligaments originate close to axis of rotation, providing smaller change in length with joint position and providing lateral stability. PIP joint ranges in only one plane, and its trochlear shape also adds to its lateral stability.
Intrinsic musculature
The intrinsic musculature, composed of the interosseous and lumbrical muscles, acts on the hand to flex the MCP joints and extend the IP joints. The interossei also act to abduct and adduct the fingers. [8] There are seven interosseous muscles: four dorsal and three (or four) volar (palmar). [9] These muscles lie on either side of the metacarpals. The dorsal interossei are abductors, whereas the volar interossei are adductors.
Each dorsal interosseous muscle, except the one lying on the ulnar side of the middle finger, has two muscle heads, one superficial and one deep. The superficial head originates most dorsally and inserts by way of a medial tendon onto the lateral tubercle at the base of the proximal phalanx. Therefore, the superficial head abducts and weakly flexes the proximal phalanx.
The deep head of the dorsal interosseous muscle forms a lateral tendon or lateral band at the base of the proximal phalanx. These lateral bands are joined by the lateral slips of the extensor tendon to form the conjoined lateral band at the level of the PIP joint.
The conjoined lateral bands on either side of the finger then join at the distal end of the middle phalanx to form the terminal extensor tendon. The terminal tendon inserts onto the base of the distal phalanx and serves to extend it. Each lateral band at the level of the middle of the proximal phalanx sends off fibers, which arch dorsally to join each other on the dorsum of the finger. These fibers flex the proximal phalanx.
Oblique (spiral) fibers also originate from the lateral bands more distally and insert onto the lateral tubercles at the base of the middle phalanx. These oblique fibers extend the middle phalanx. Therefore, the deep head of the dorsal interosseous muscle acts to flex and weakly abduct the proximal phalanx and extend the middle and distal phalanges.
The volar interossei each only have one muscle head and form the ulnar lateral band of the index finger and the radial lateral band of the ring and little finger.
The hypothenar muscles function similarly to the interossei for the small finger. The abductor digiti quinti (ADQ) function is similar to that of the superficial head of a dorsal interosseous muscle. The flexor digiti quinti brevis (FDQB) functions similarly to the deep head of a dorsal interosseous muscle, forming the ulnar lateral band. The opponens digiti quinti (ODQ) is a third hypothenar muscle that serves to flex and supinate the fifth metacarpal.
The lumbrical muscles arise from the flexor digitorum profundus (FDP) tendons in the palm and join the radial lateral band at the middle of the proximal phalanx. The lumbricals extend the PIP and distal IP (DIP) joints and assist in flexing the MCP joints.
Volar plate anatomy
Architectural differences exist between the volar plates of the MCP and IP joints. The MCP volar plate is composed of crisscrossing bands of fibers that collapse like an accordion on flexion and expand with extension. [10] The IP volar plate is a more rigid cartilaginous structure that does not collapse but glides with movement. It is attached to the proximal phalanx only by the proximal checkrein ligaments; therefore, the rigid IP volar plate can slide proximally and distally with joint motion to protect the joint. (See the image below.)
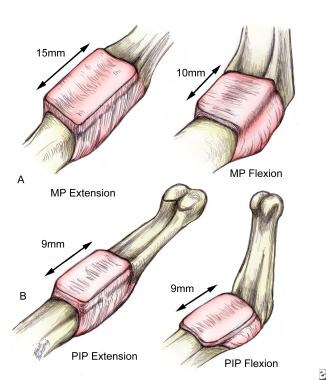 Architectural differences exist between volar plates of metacarpophalangeal (MCP) and interphalangeal (IP) joints. MCP volar plate is composed of crisscrossing bands of fibers that collapse like accordion on flexion and expand with extension. IP volar plate is more rigid cartilaginous structure that does not collapse but glides with movement. It is attached to proximal phalanx only by proximal checkrein ligaments; therefore, rigid IP volar plate can slide proximally and distally with joint motion to protect joint.
Architectural differences exist between volar plates of metacarpophalangeal (MCP) and interphalangeal (IP) joints. MCP volar plate is composed of crisscrossing bands of fibers that collapse like accordion on flexion and expand with extension. IP volar plate is more rigid cartilaginous structure that does not collapse but glides with movement. It is attached to proximal phalanx only by proximal checkrein ligaments; therefore, rigid IP volar plate can slide proximally and distally with joint motion to protect joint.
Pathophysiology
Edema is the initial response to any insult to the hand and leads to adverse sequelae. Joint stiffness develops as intra-articular hematoma and fluid accumulate within the synovial space, distending the capsule. Increased fluid content within the articular capsule and collateral ligaments effectively shortens these structures, favoring extension. The fluid in the joint space also hydraulically drives the MCP joints into extension.
In extension, the joint is able to accommodate this increased fluid capacity. As the MCP joints extend, the flexor tension on the IP joints increases and the extensor tension decreases. This causes the PIP and DIP joints to flex. The resultant late deformity is the intrinsic negative (or minus) hand, consisting of MCP joint extension, IP joint flexion, thumb adduction, and wrist flexion.
With injury, checkreins form at the IP joints (see the image below). Checkreins are collagenous bands connecting the lateral sides of the proximal volar plate to the assembly lines on the volar lateral surfaces of the phalanx. Assembly lines are the two ridges along the volar lateral surfaces of the phalanx, to which are attached volar ligamentous structures such as the flexor sheath, the Cleland and Grayson ligaments, and the oblique retinacular ligaments of Landsmeer.
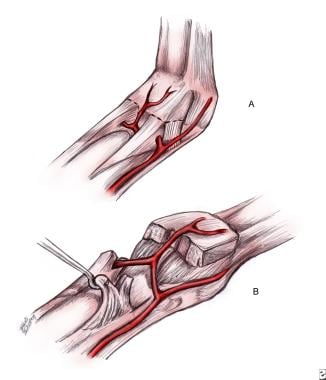 With injury, checkreins form at IP joints. Checkreins are collagenous bands connecting lateral sides of proximal volar plate to assembly lines on volar lateral surfaces of phalanx. Assembly lines are two ridges along volar lateral surfaces of phalanx to which are attached volar ligamentous structures (eg, flexor sheath, Cleland and Grayson ligaments, and oblique retinacular ligaments of Landsmeer).
With injury, checkreins form at IP joints. Checkreins are collagenous bands connecting lateral sides of proximal volar plate to assembly lines on volar lateral surfaces of phalanx. Assembly lines are two ridges along volar lateral surfaces of phalanx to which are attached volar ligamentous structures (eg, flexor sheath, Cleland and Grayson ligaments, and oblique retinacular ligaments of Landsmeer).
The volar plate pocket behind the MCP volar plate is smaller than that at the IP joint, and checkreins do not develop at the MCP joint (see the image above). [10]
Compartment syndrome is the usual cause of posttraumatic intrinsic contractures owing to edema and ischemia. Hematoma and edema fill the interosseous muscle compartment and are trapped by the firm dorsal and volar interosseous fascia. [11] Capillary compression and venous stasis add to the congestion. As the edema subsides, fibrosis develops.
Compressive circular dressings can also impede venous drainage and lead to the development of myostatic contractures in the interossei. Finally, muscle necrosis and fibrosis may ensue with cases of severe and prolonged deep-space edema of the hand.
Etiology
Excessive immobilization, trauma, inflammation, infection, tumor, central nervous system (CNS) disease, and joint destruction are all causes of joint stiffness and intrinsic contractures. [12, 13] Decreased blood supply to the hand as a result of injury or primary disease of the vessels of the upper extremity is a leading cause of intrinsic muscle contracture.
Prognosis
The prognosis for each patient is variable and depends on the severity of the contracture and the underlying cause of the contracture. The surgeon's objective is to restore structure and function to the contracted hand. The ultimate goal is to provide the patient maximal comfort and functional independence.
-
Metacarpal head is uniquely shaped: ovoid in sagittal plane and widening from dorsal to volar dimension. Collateral ligaments are eccentrically mounted dorsal to axis of rotation of metacarpophalangeal joint. This anatomy causes variable degrees of tightness on collateral ligaments based on position of joint via camlike effect. When joint is in extension, collateral ligaments are lax; in flexion, collateral ligaments span greater distance and are tight.
-
Proximal interphalangeal (PIP) joint collateral ligaments originate close to axis of rotation, providing smaller change in length with joint position and providing lateral stability. PIP joint ranges in only one plane, and its trochlear shape also adds to its lateral stability.
-
Architectural differences exist between volar plates of metacarpophalangeal (MCP) and interphalangeal (IP) joints. MCP volar plate is composed of crisscrossing bands of fibers that collapse like accordion on flexion and expand with extension. IP volar plate is more rigid cartilaginous structure that does not collapse but glides with movement. It is attached to proximal phalanx only by proximal checkrein ligaments; therefore, rigid IP volar plate can slide proximally and distally with joint motion to protect joint.
-
With injury, checkreins form at IP joints. Checkreins are collagenous bands connecting lateral sides of proximal volar plate to assembly lines on volar lateral surfaces of phalanx. Assembly lines are two ridges along volar lateral surfaces of phalanx to which are attached volar ligamentous structures (eg, flexor sheath, Cleland and Grayson ligaments, and oblique retinacular ligaments of Landsmeer).







