Practice Essentials
Fixed contractures of the intrinsic muscles may severely impair the function of the hand. A mild contracture may inhibit certain hand functions without any gross deformity. The patient may complain of a weak grip when using, for example, a screwdriver or a hammer. Severe contractures cause metacarpophalangeal (MCP) joint flexion and interphalangeal (IP) joint extension, resulting in an intrinsic-plus deformity. The patient experiences difficulty in grasping, pinching, and abducting the fingers. In combination with sensory loss, the hand is severely disabled.
Individual involvement of intrinsic muscles results in characteristic deformities. [1] Lumbrical contracture causes finger extension while the patient is trying to flex the finger. The origin of the lumbrical is pulled proximally with extrinsic flexion, and the IP joints are extended. Contraction of the abductor digiti minimi (ADM) presents as small-finger abduction and causes MCP joint flexion and IP joint extension. Thenar intrinsic muscle contracture can cause thumb adduction, MCP joint flexion, and IP joint hyperextension. The patient loses effective pinch, large-volume grip, and hand dexterity.
Intrinsic and extrinsic tightness may coexist in the same patient. Intrinsic contracture may not be clinically apparent until associated extrinsic changes are corrected. In cases of extrinsic tightness, proximal IP (PIP) joint flexion increases when the MCP joint is extended and decreases when the MCP joint is flexed. It should be kept in mind that the ability to flex PIP joints does not exclude intrinsic contracture. PIP flexion should be evaluated while the MCP joint is extended.
Intrinsic tightness or contractures should initially be treated conservatively. Such treatment includes hand therapy and splinting to increase the effective range of motion (ROM) and prevent fixed contractures. When appropriate hand therapy does not correct the disability, the following surgical options may be considered:
-
Opponensplasty
-
Palmaris longus opponensplasty
-
Crossed intrinsic transfer
-
Bunnell lateral band tenotomy
-
Littler distal intrinsic release
-
Intrinsic tenodesis
-
Spiral oblique retinacular ligament (SORL) construction
-
Interosseous slide
-
Lumbrical release
-
PIP joint arthrodesis with intrinsic muscle release
-
Thumb intrinsic slide or excision
-
Zancolli lasso procedure
-
Fowler technique
Hand compartment syndrome should be treated promptly.
Anatomy
Muscles of hand
Normal positioning and movement of the digits depends on the functional integrity of extrinsic and intrinsic muscles. The extrinsic muscles originate in the forearm, and the intrinsic muscles originate distal to the wrist. The intrinsic muscles [2] are traditionally divided into five groups (or four, if the interossei are grouped together), as follows:
-
Thenar
-
Hypothenar
-
Palmar (volar) interossei [3]
-
Dorsal interossei
-
Lumbricals
The four thenar muscles are as follows:
-
Abductor pollicis brevis (APB)
-
Flexor pollicis brevis (FPB)
-
Opponens pollicis
-
Adductor pollicis
The APB abducts the thumb away from the palm. The FPB flexes the thumb MCP joint. The opponens pollicis abducts, flexes, and pronates the first metacarpal. With these muscles, the thumb is brought from lateral to medial position across the palm in opposition to the four ulnar digits. The adductor pollicis adducts the thumb toward the palm.
The three hypothenar muscles are as follows:
-
ADM
-
Flexor digiti minimi brevis (FDMB)
-
Opponens digiti minimi (ODM)
The ADM abducts the little finger away from the fourth finger. The FDMB flexes the little finger at the MCP joint. The ODM abducts, flexes, and supinates the fifth metacarpal. With these muscles, the little finger is brought into opposition to the thumb.
Most anatomists describe three palmar interosseous muscles and four dorsal interosseous muscles. The dorsal interossei flex the MCP joints and extend the IP joints. The dorsal interossei also abduct the four ulnar digits from one another; the palmar interossei adduct the four ulnar digits together toward the third finger.
The four lumbrical muscles function as a connection between the flexor digitorum profundus (FDP) and the extensor mechanism. Their main function is to facilitate extension of the IP joints. The lumbricals can extend the IP joints in any position of the MCP joints.
Nerves of hand
The ulnar nerve innervates most of the intrinsic muscles in the hand: all seven interossei, the three hypothenar muscles, the adductor pollicis, the deep head of the FPB, and the two ulnar lumbricals. All of the remaining intrinsic muscles—that is, the two radial lumbricals, the APB, the opponens pollicis, and the superficial head of the FPB—are thus innervated by the median nerve. [4] (See Table 1 below.)
Table 1. Muscles of Forearm (Open Table in a new window)
Muscle |
Nerve Supply |
| Muscles of anterior fascial compartment | |
Pronator teres |
Median nerve |
Flexor carpi radialis |
Median nerve |
Palmaris longus |
Median nerve |
Flexor carpi ulnaris |
Ulnar nerve |
Flexor digitorum superficialis |
Median nerve |
Flexor pollicis longus |
Anterior interosseous branch of median nerve |
Flexor digitorum profundus |
Ulnar and median nerves |
Median nerve supplies index and middle fingers in 75% of patients; ulnar nerve supplies middle, ring, and little fingers in 75% of patients (therefore, the middle finger has dual innervation in 75% of patients) |
|
Pronator quadratus |
Anterior interosseous branch of median nerve |
Muscles of lateral fascial compartment |
|
Brachioradialis |
Radial nerve |
Extensor carpi radialis longus |
Radial nerve |
Muscles of posterior fascial compartment |
|
Extensor carpi radialis brevis |
Deep branch of radial nerve |
Extensor digitorum |
Deep branch of radial nerve |
Extensor digiti minimi |
Deep branch of radial nerve |
Extensor carpi ulnaris |
Deep branch of radial nerve |
Anconeus |
Radial nerve |
Supinator |
Deep branch of radial nerve |
Abductor pollicis longus |
Deep branch of radial nerve |
Extensor pollicis brevis |
Deep branch of radial nerve |
Extensor pollicis longus |
Deep branch of radial nerve |
Extensor indicis |
Deep branch of radial nerve |
Muscles of hand lumbricals |
|
Two radial lumbricals |
Median nerve |
Two ulnar lumbricals |
Ulnar nerve |
Interossei |
Ulnar nerve |
Abductor pollicis brevis |
Median nerve |
Flexor pollicis brevis |
Median nerve |
Opponens pollicis |
Median nerve |
Adductor pollicis |
Ulnar nerve |
Abductor digiti minimi |
Ulnar nerve |
Flexor digiti minimi brevis |
Ulnar nerve |
Opponens digiti minimi |
Ulnar nerve |
Pathophysiology
Median nerve injury
Median nerve injuries are commonly referred to as high (ie, at or above the elbow) or low (ie, distal forearm to midforearm). Whereas a high injury affects both extrinsic and intrinsic motor function, a low injury affects only intrinsic motor function.
A high median nerve division paralyzes the extrinsic muscles: pronator teres, flexor carpi radialis (FCR), palmaris longus, flexor digitorum superficialis (FDS), flexor pollicis longus (FPL), radial half of the FDP, and pronator quadratus. As a result, the forearm tends to rest in supination with the wrist in ulnar deviation. The median-innervated intrinsic muscles are also paralyzed. The lumbricals to the index and long fingers are paralyzed. Therefore, only weak flexion of the MCP joints is possible with the ulnar-innervated interossei. [5, 6, 7]
The IP joints of the thumb and the index and middle fingers cannot flex, as a result of paralysis of the FDP and FDS motor units. If the ulnar nerve supplies the FDP to the ring finger, the ring finger IP joints can then flex. The ulnar nerve supplies the FDP motor units to the ring and little fingers, so that the fourth and fifth fingers can flex. The APB and the opponens pollicis are paralyzed. The thumb rests in the plane of the palm and cannot be positioned for a pulp-to-pulp pinch between the thumb and fingers. The thumb IP joint is extended because of paralysis of the FPL.
Median nerve injury at the wrist preserves extrinsic muscle function. The pronator teres, FDS, FDP, and FPL motor units are intact. The first two lumbricals, the APB, and the opponens pollicis are paralyzed. When the patient slowly makes a fist, the index and middle fingers clearly lag behind the fourth and fifth fingers because of a lack of initiation of flexion at the MCP joints by the lumbricals. The thumb rests in the plane of the palm and cannot oppose the fingers (see the image below). The patient can flex the thumb terminal phalanx because the FPL is not paralyzed.
 Intrinsic muscles innervated by median nerve (abductor pollicis brevis and opponens pollicis) are checked by resisting palmar abduction of thumb.
Intrinsic muscles innervated by median nerve (abductor pollicis brevis and opponens pollicis) are checked by resisting palmar abduction of thumb.
Ulnar nerve injury
Ulnar nerve lacerations are commonly referred to as high or low to reflect whether the injury affects extrinsic and intrinsic muscles. [6, 8, 9, 10]
High ulnar nerve injury results in paralysis of the flexor carpi ulnaris (FCU) and the ulnar half of the flexor FDPs, generally FDPs III-V. The distal phalanges of the fourth and fifth fingers cannot flex. Because the FDP motor units have a common origin, some weak flexion of the fourth and fifth fingers may be possible even if the ulnar half is supplied by the ulnar nerve. An attempt to flex the wrist results in radial deviation due to paralysis of the FCU.
All seven interossei, the third and fourth lumbrical muscles, the adductor pollicis, generally one head of the FPB, and all three hypothenar muscles (FDMB, ADM, and ODM) are paralyzed. The patient cannot adduct or abduct the fingers. If the examiner places a piece of paper between the patient's fingers, he or she cannot hold it when the paper is pulled away.
The MCP joints are hyperextended, and the IP joints are flexed. These changes are more obvious at the ring and little fingers, because the first and second lumbrical muscles are not paralyzed. This condition is called a claw-hand deformity. [11] The thumb can weakly adduct through the extensor pollicis longus (EPL). The patient can pinch and hold a paper between the thumb and index finger by strongly flexing the IP joint with the FPL. The combination of strong IP and weak MCP flexion is called the Froment sign.
Ulnar nerve injury at the wrist spares the FCU and the medial half of the FDPs. The patient can flex the wrist and all the distal IP (DIP) joints. However, all intrinsic muscles innervated by the ulnar nerve are paralyzed, and both the claw-hand deformity and the Froment sign (see the image below) are prominent.
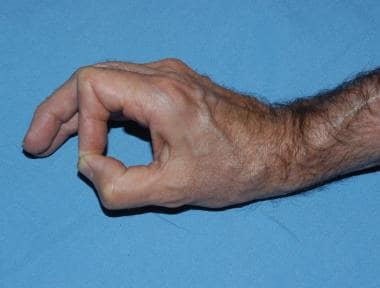 Image from patient with ulnar neuropathy demonstrates Froment sign during pinching. Loss of ulnar-innervated adductor pollicis results in reliance on flexor pollicis longus and exaggerated interphalangeal (IP) joint flexion. Loss of metacarpophalangeal (MCP) joint flexor leads to MCP hyperextension over time.
Image from patient with ulnar neuropathy demonstrates Froment sign during pinching. Loss of ulnar-innervated adductor pollicis results in reliance on flexor pollicis longus and exaggerated interphalangeal (IP) joint flexion. Loss of metacarpophalangeal (MCP) joint flexor leads to MCP hyperextension over time.
Etiology
Open or closed trauma is the most frequent cause of intrinsic hand deformities. [12, 13] Intrinsic muscle contracture can also be caused by inflammation, tumor, central nervous system (CNS) disease, joint destruction, leprosy (Hansen disease), compartment syndrome, or rheumatoid disease. Prolonged immobilization in a tight cast or splint can cause intrinsic muscle tightness.
Although sensory loss contributes to the overall impairment, it does not contribute to the deformity. Ulnar nerve compression can occur at the elbow (the cubital tunnel) or at the wrist (in the Guyon canal) and can lead to degeneration of intrinsic hand muscles. [14] Median nerve compression associated with intrinsic loss can occur with pronator syndrome or carpal tunnel syndrome. Anterior interosseous nerve compression does not result in intrinsic loss, because this nerve innervates only the extrinsic motor units.
Epidemiology
The most common cause of intrinsic hand deformities is trauma.
One third of all patients with rheumatoid arthritis (RA) develop some degree of intrinsic contracture during the course of their disease. Hand deformities tend to progress in RA. [15]
Peripheral nerve palsy, most commonly afflicting the ulnar nerve at the elbow, occurs in 20-25% of patients with leprosy. Claw hand due to ulnar nerve paresis is therefore the most common presentation in this group of patients.
-
Intrinsic muscles innervated by median nerve (abductor pollicis brevis and opponens pollicis) are checked by resisting palmar abduction of thumb.
-
Image from patient with ulnar neuropathy demonstrates Froment sign during pinching. Loss of ulnar-innervated adductor pollicis results in reliance on flexor pollicis longus and exaggerated interphalangeal (IP) joint flexion. Loss of metacarpophalangeal (MCP) joint flexor leads to MCP hyperextension over time.
-
Ulnar-innervated intrinsic muscles can be checked by resisting abduction of index (first dorsal interosseous muscle) and small fingers (abductor digiti minimi).
-
Gloved examiner checks for intrinsic tightness. With metacarpophalangeal (MCP) joint hyperextended, proximal interphalangeal (PIP) joint is passively flexed. Intrinsic muscles are volar to axis of rotation of MCP joint and dorsal to axis of PIP joint. MCP joint hyperextension tightens intrinsics. Results of this test are compared with those in contralatera, normal hand. Note intrinsic atrophy in first dorsal web space.
-
Image from patient with partial ulnar nerve paralysis who is asked to extend digits. Hyperextension of metacarpophalangeal (MCP) joints of ring and small fingers occurs with loss of intrinsic ulnar-innervated MCP flexors. Index and middle fingers have median-innervated intrinsics (lumbricals) that allow extrinsics to extend interphalangeal (IP) joints.
-
When examiner prevents metacarpophalangeal (MCP) hyperextension of ring and fifth fingers, patient can completely extend interphalangeal (IP) joints with extrinsic tendons.




